The Comprehensive Guide for EpiPens
The EpiPen is an epinephrine auto-injector that delivers a single, fixed dose of adrenaline in the event of a severe allergic reaction or anaphylaxis. These life-saving devices are essential for individuals who are at risk of these serious allergic reactions, and it is crucial to know how to administer them correctly in case of emergency.
Continue reading to discover more about anaphylaxis, an overview of EpiPens, and a guide to administering the adrenaline auto-injector alongside anaphylaxis first aid.
The EpiPen is one of two types of adrenaline auto-injectors available in Australia to treat severe allergic reactions and anaphylaxis. It provides a single, fixed dose of adrenaline via intramuscular injection into the muscle of the leg. EpiPens can be administered by anyone, including those without medical training or even self-administered, and reduces the risk of hospitalization and even death if administered early enough.
Adrenaline is a natural hormone produced by the body and is released in response to an anaphylactic event. An injection of adrenaline assists this response and combats the anaphylactic symptoms by inducing vasoconstriction, which is the narrowing of the blood vessels, to combat low blood pressure and bronchodilation, the relaxation of the airways to improve breathing.
There are three types of EpiPen available:
Individuals who have been identified as having a risk of anaphylaxis should always carry an adrenaline auto-injector. It is also recommended that adrenaline auto-injectors, such as the EpiPen, should be carried in schools, childcare education centres, and other non-medical centres to avoid delays in administering adrenaline in the event of anaphylaxis.
When the immune system perceives a substance as harmful, it can trigger an allergic reaction that can range from mild to life-threatening. Anaphylaxis is an extreme form of allergic reaction that can occur when the body identifies an allergen as a danger and triggers the release of a chemical called Histamine. This chemical can cause severe responses, including the widening of blood vessels (vasodilation) that can lead to a sudden drop in blood pressure and an irregular heartbeat. It can also cause narrowing of the airways (bronchoconstriction) which can make it difficult to breathe and lead to pulmonary edema, where fluid accumulates in the lungs and causes further swelling.
While the substance may be harmless to most people, those who are susceptible to severe allergic reactions need to be aware of the potential dangers and take appropriate precautions.
Exposure to allergens can lead to a range of symptoms, from mild to severe, including anaphylaxis. Mild symptoms of an allergic reaction may include:
On the other hand, severe allergic reactions and anaphylaxis can result in:
Anaphylaxis can occur as soon as a few minutes or up to two hours after exposure to the allergen. If someone experiences severe symptoms, immediate first aid should be given, and emergency medical attention should be sought.
Anaphylaxis can be triggered by a variety of allergens, some of which are more common than others. This can include:
In some cases, the cause of anaphylaxis cannot be identified despite extensive testing, which is referred to as ‘idiopathic anaphylaxis.’
If you or someone you know has a history of serious allergies or has experienced anaphylaxis in the past, it is important to take precautions such as identifying triggers through allergy testing, avoiding allergens where possible, and always carrying an adrenaline auto-injector.
Individuals diagnosed with a severe allergy and at risk of anaphylaxis should carry an auto-injector at all times. In the event of an anaphylactic reaction, immediate administration of an adrenaline auto-injector, such as an EpiPen, is necessary.
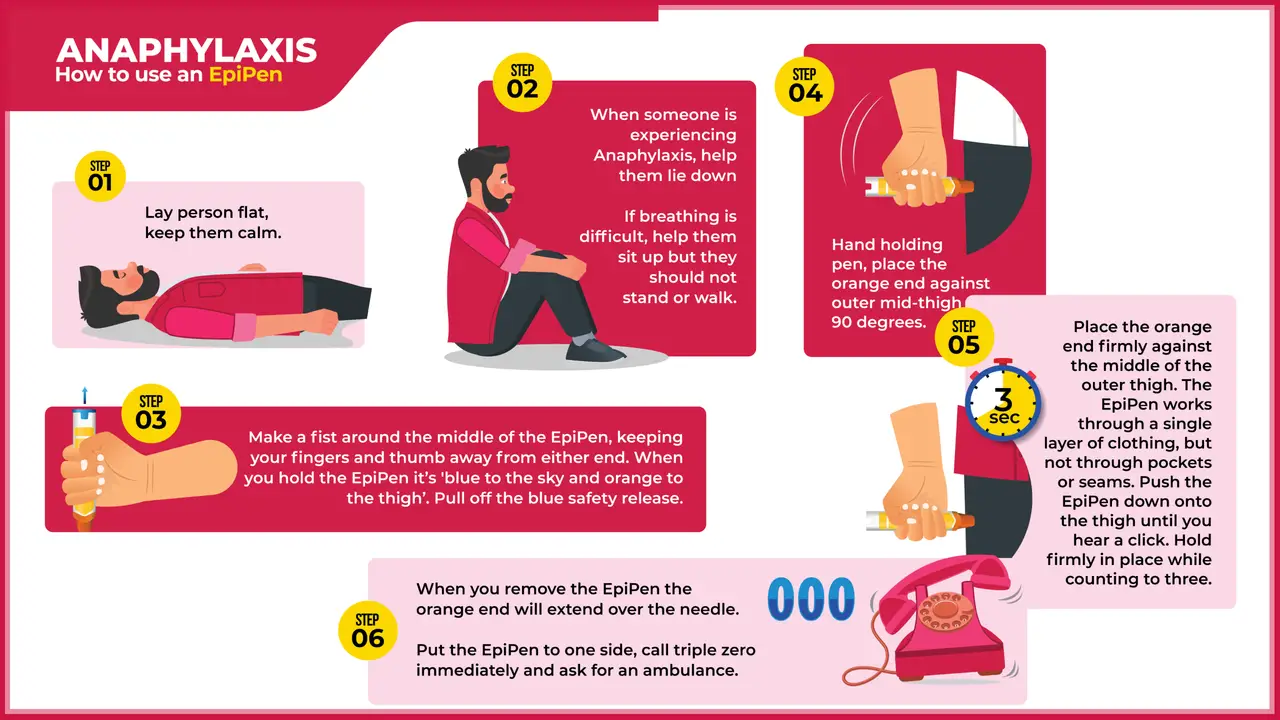
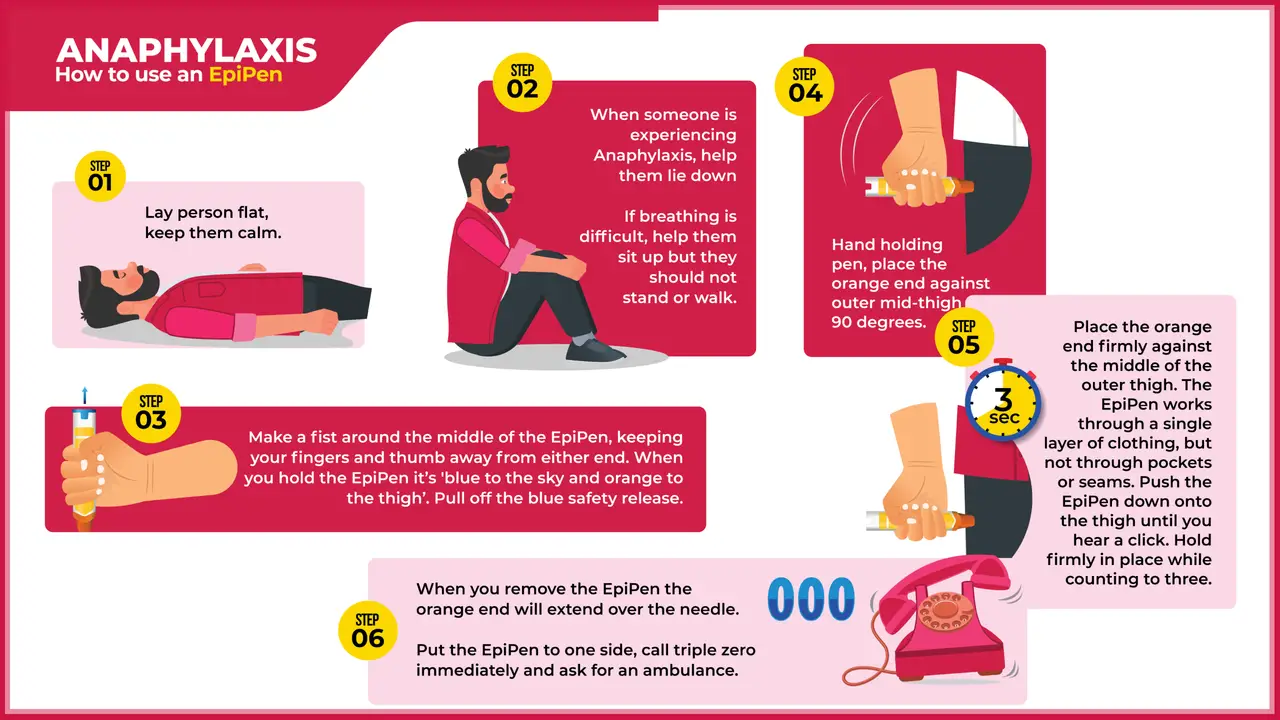
There are three simple steps to administering an EpiPen:
Record the time of administration and keep the EpiPen to provide to the ambulance or medical professionals. The person may still look unwell after administering due to the temporary side effects of adrenaline such as elevated heart rate, trembling, and paleness. It is important that after administering the EpiPen, the person should never take a shower. Warm showers promote vasodilation which can cause the person’s blood pressure to drop further and potentially faint or fall.
If you are unsure if a person at risk of anaphylaxis is experiencing an anaphylactic event, it is best to administer the EpiPen anyway. It is more harmful to under-treat and it becomes a potentially life-threatening situation as opposed to over-treating mild to moderate symptoms.
EpiPens need to be checked regularly to ensure they have not expired or the adrenaline has not discoloured. If there are no in-date devices available, it is best to use the most recently expired auto-injector available knowing that it can help but may not be as effective as an in-date device.
In addition to administering the EpiPen, anaphylaxis first aid should be administered which includes:
For more information on administering adrenaline to treat anaphylaxis, explore our Anaphylaxis and Adrenaline Guide Sheet.
The EpiPen is an essential device that can save lives in cases of anaphylaxis. It is essential not only to recognise the signs and symptoms of anaphylaxis but also to have a clear understanding of how to properly use an EpiPen for effective administration. By being adequately informed and prepared, you can have the confidence to handle a severe allergic reaction or anaphylaxis, avoiding, any potential errors that may result in serious consequences.
To learn more about treating anaphylaxis as well as first aid for other emergency medical situation, enrol in one of our first aid courses near you:
October 2, 2013
In an asthma or anaphylaxis emergency you should know the symptoms, remove triggers, and know how to respond. Read on to understand these important aspects in the context of such an emergency.
May 7, 2024
Asthma, a chronic respiratory condition affecting millions worldwide, is often shrouded in myths and misconceptions. Despite how common it is, there is a distinct lack of common knowledge. This is leading to potential mismanagement and unnecessary anxiety for those living with asthma.

February 19, 2024
For many Australians, our city and outdoor lifestyles come with a hidden challenge – dust allergies. Dust mites, pollen, and other airborne particles can trigger allergic reactions, affecting a significant portion of the population.